By Eric Maina Kamau
Health Economist & Marketing Researcher
Bshrmlmr301422@spu.ac.ke
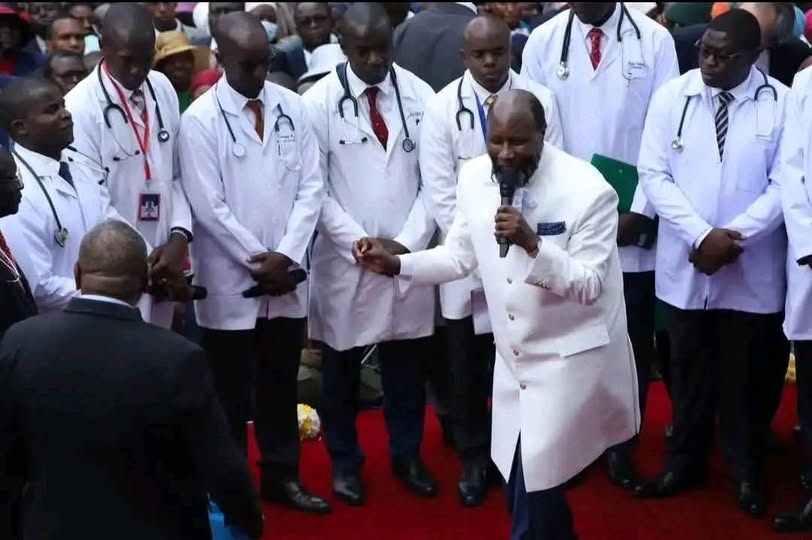
Testimonies by medical doctors at Prophet David Owuor’s Nakuru rally have triggered a nationwide debate at the intersection of religion, science, and ethics. During the event, several clinicians claimed that prayer had cured HIV and other chronic illnesses. Circulated widely through viral social media clips, these assertions have inspired hope among some believers while raising serious concern among health professionals and regulators.
As a health researcher, I acknowledge the significant role faith plays in providing comfort, resilience, and community support. Spiritual practices can offer measurable psychological benefits, including stress reduction and improved coping mechanisms. However, when licensed medical practitioners publicly endorse unverified cures, the implications for public health are profound. Kenya has made substantial investments in HIV treatment, with antiretroviral therapy (ART) transforming the disease into a manageable condition. Claims that prayer alone can replace ART risk undermining decades of progress and may prompt patients to abandon lifesaving medication.
This challenge is not unique to Kenya. Globally, faith-healing controversies have surfaced in countries such as South Africa, Nigeria, and the United States, where religious leaders have claimed miraculous cures for HIV, cancer, or COVID-19. In South Africa, unverified claims of “spiritual healing” contributed to delays in ART uptake in the early 2000s, exacerbating the epidemic. In the United States, faith-healing movements have at times clashed with medical authorities over vaccination, leading to outbreaks of preventable diseases. These examples underscore the dangers of conflating spiritual belief with medical treatment.
The Nakuru debate also highlights the influence of social media in shaping public discourse. Platforms such as Twitter amplified both praise and outrage, quickly turning the rally into a national flashpoint. While faith communities deserve respect, medical professionals bear a distinct responsibility: to protect patients from harm and ensure that hope is anchored in scientific evidence. In this context, scrutiny by regulatory bodies such as the Kenya Medical Practitioners and Dentists Council is both appropriate and necessary to determine whether professional boundaries were breached.
The broader lesson from Nakuru is not a rejection of faith, but a call for balance. Faith can inspire and sustain, but it must complement—rather than replace—medical care. Medicine safeguards lives through evidence-based practice. Kenya’s public health future will depend on how effectively the country navigates this delicate intersection of belief, science, and professional responsibility.